How does a reflux esophagitis manifest itself?
A reflux esophagitis, also called reflux disease or GERD: gastroesophageal reflux, is the name for an inflammation of the esophagus, caused by the backflow of stomach contents into the esophagus. A typical sign of GERD is the heart-burn, a burning pain behind the sternum or within the upper abdomen, especially after lying down or after meals. Furthermore a feeling of pressure behind the sternum can occur without causing pain. Additional symptoms are such as the eructation of air, flatulences, difficulties while swallowing, eructation of food remnants (regurgitation), nausea, salty taste within the mouth, teeth damages (caries) and bad breath. Beyond that, reflux can lead to arrhythmia, chesty cough (inflammation of the bronchia, or increased asthma caused by reflux), hoarseness (laryngitis caused by reflux) and cause insomnia.
What causes an inflammation of the esophagus?
After the consumption of a meal, the food is lead from the mouth to the esophagus, then to the stomach. Within the stomach, gastric juices decompose the food. The transition between esophagus and the stomach is called cardia. That is where inside of the middle layer of the wall there is a sphincter muscle, called low esophageal sphincter (LES), which usually avoids a backflow of food and gastric juices into the esophagus. The sphincter muscle is located in height of the diaphragm, which divides ribcage cavity and abdominal cavity. A regurgitation may also appear in case of a malfunction of the movement of the oesphagus-muscles, an absent atony of the LES during the act of swallowing ( called achalasy) The opening in the diaphragm is usually that small, that it only allows the gullet to pass through and thereby stomach is fastend in the abdominal cavity. If an expansion of the opening should take place, the stomach sildes into the ribcage, which is called adiaphragmatic hernia/ hiatus hernia. Due to the fact that in this case, the function of the LES is no longer supported, the gastroesophageal reflux disease occurs in 10% of the cases.
Further contributive factors are: overweight, pregnancy, late consumption of food, alcohol and coffee.
How is the diagonsis made?
Eventhough the symptomes already indicate the disease, a gastroscopy is needed to exclude other sicknesses like cancer, before initiating the theraphy. This examination is performed ambulant, whithout causing pain, supported by suitable medicaments. As the circumstances require further examinations, like taking an x-ray with contrastmedium in the gullet, computed tomography, longterm pH-metrie and Ösphagus- Manometrie, can become relevant.
What forms of diaphragmatic hernia are known?
Usually the gastric bubble and the gullet build an sharp angle, called His- angle. In case of a deformation this angle is obtuse. The axial hiatus hernia, called sliding hernia, ist the most common form of the diaphragmatic hernia. In this situation the upper part of the stomach and the cardia slide through the widder hole of the diaphragm into the ribcage. More than 50% of the people in the age over 50 are affected by this situation.In case of a paraesophagal (rolling) hernia the LES remains in the correct position, however a part of the stomach slides besides the gullet through the hernial orifice into the ribcage. This situation might lead to a strangulation oft he stomach, with disturbances of the passage, ulcers and anaemia. An advanced stage of this form is called upside- down- stomach. In this situation the entire stomach is located within the ribcage. Forms that combine the axial and the paraesophageal hernia do also excist. An upside-down stomach is most of the time a combined form of the diaphragmatic hernia.
Which complications may occur in virtue of a reflux disease?
In consequence of the GERD ailment, ulcers might develop in the gullet, in very few cases hemmorhages or tresspassing of gastric contents into the lung (aspiration) appears, and leads to a restriction of the gullet. 5% of GERD patients develop a Barret- syndrom. In that case, the regular squamous epithelium of the inside layer of the gulletis replaced to a columnar configuration. This phenomenon is called metaplasy. A Barrett’s esophagus is a prestage of cancer. The risk of adenocarcinoma (esophageal cancer) for long-segment-Barret ( over 3 cm) is estimated about 0,5% per year.
When is a surgery necessary?
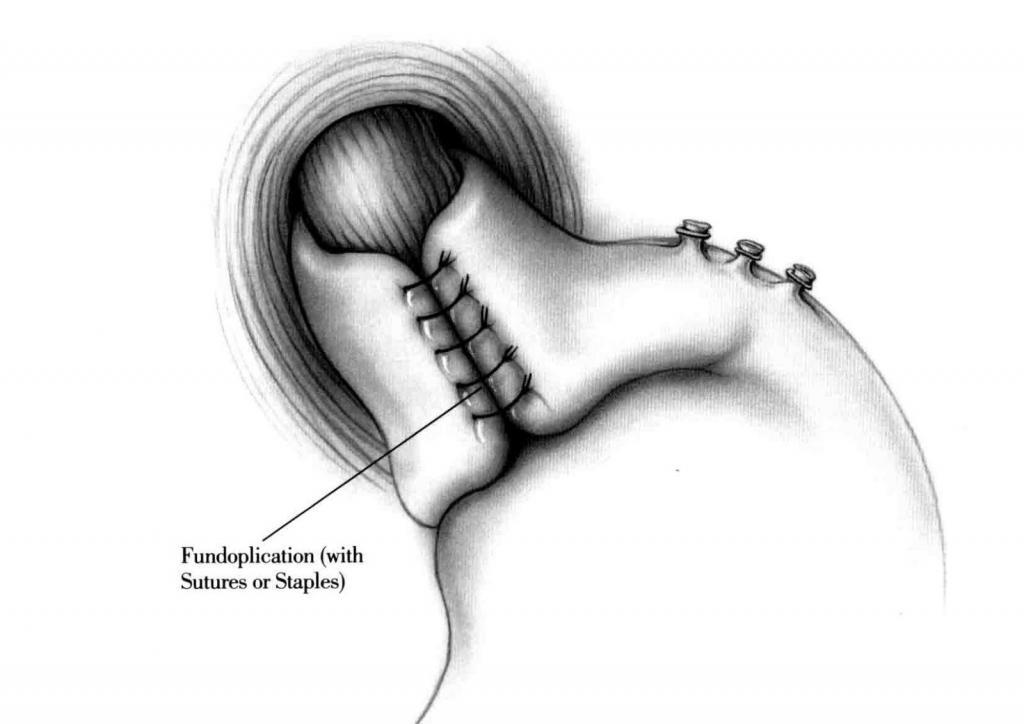
General measures, like weight reduction, avoiding late eating, loose clothing and sleeping with an elevated head, may ease minor reflux afflictions. If the afflictions should still occur or a gastroscopycally proofed gastroesophageal reflux is validated, a medical treatment with proton pump inhibitors (PPI) is needed. In most of the cases, the symptoms are eased by that therapy. In advanced stages, with nonexsisting effect or intolerance of the medicaments, in case of aspiration or biliary reflux – a surgery is indicated. Likewise in the case of paraesophageal hernia, because of the risk of complications an operative treatment is necessary. The accurate positions of the stomach and the function of the lower LES can only be reconstructed by surgical treatment. The surgery is performed minimal invasive by using 4-5minor cuts (5-11 mm) in the skin. After the correction of the stomach position, the hiatal orificeis being constrained (hiatal plasty), furthermore a part of the stomache is wraped around the lower part of the gullet (fundoplication),thereby the function of the LES is being supported. In addition the stomach is being attached to the diaphragm (gastropexy). The surgergy takes about 1 hour. The patient is allowed to drink at the day of the intervention and the buildup of regular food starts the day after. The stay at the hospital takes 3 to 4 days.
press report
